What No One Tells You About Midlife Hormones
If you’re in your 40s or 50s, you’ve likely heard of menopause, but what’s often left out of the conversation is how the hormonal changes during perimenopause can impact nearly every aspect of your life: your energy, mood, sleep, and even your memory.
Grasping what’s happening with your hormones during this time can be the key to feeling like yourself again.
What Is Perimenopause?
Perimenopause is the natural transition leading up to menopause, typically starting in your 40s, though it can begin as early as your mid-30s. This phase is marked by fluctuating hormone levels, particularly estrogen and progesterone, as ovarian function gradually declines. These hormonal shifts can lead to irregular periods, changes in cycle length, and a wide range of physical and emotional symptoms. Perimenopause can last anywhere from 4 to 10 years, varying from woman to woman, and ends when you’ve gone 12 consecutive months without a period, signaling the official arrival of menopause. This marks the end of ovarian activity and the start of sustained lower levels of estrogen and progesterone.
One symptom that’s often overlooked in perimenopause is joint pain, especially in the shoulders and hips. This discomfort is linked to fluctuating estrogen levels. Estrogen plays a protective role in joint health, so as levels drop, you may notice more stiffness, soreness, or swelling. On top of that, midlife is also the time when natural wear and tear on the joints starts to become more noticeable.
It’s Not Just About Hot Flashes
Hot flashes are the classic symptom we often associate with perimenopause and menopause, but there’s so much more happening. Hormonal fluctuations can affect your energy, focus, metabolism, sleep, and even your sense of well-being.
As you transition through perimenopause (which can start as early as your mid-30s), your body begins to experience hormonal imbalances. Estrogen and progesterone are two of the key hormones that begin to fluctuate, often resulting in an unpredictable rollercoaster ride of symptoms.
Here are a few things you might not know about the role these hormones play:
Estrogen: More Than Just a Reproductive Hormone
Estrogen is often thought of as the primary hormone responsible for regulating the menstrual cycle and supporting fertility, but its influence extends far beyond the reproductive system. In fact, estrogen plays a critical role in multiple systems throughout your body
Brain Health and Cognitive Function
Estrogen has a direct impact on the brain. It’s not just about managing mood swings (although it does that); estrogen also supports cognitive functions such as memory, learning, and concentration. This is why many women report experiencing "brain fog" during perimenopause and menopause, fluctuating estrogen levels can make it harder to focus and remember things.
Estrogen has been shown to help protect brain cells and promote neuroplasticity (the brain's ability to adapt and form new connections). As estrogen levels decline, some women may experience an increase in memory issues, difficulty concentrating, or even anxiety. This is often compounded by poor sleep or increased stress levels, which are also influenced by estrogen.
Mood Regulation
Estrogen plays a key role in neurotransmitter regulation, specifically in the production of serotonin (the "feel-good" hormone) and dopamine (the "motivation" neurotransmitter). When estrogen levels dip, as they do during perimenopause, serotonin production can suffer. This can lead to feelings of irritability, anxiety, and even depression.
Studies have shown that women who experience higher levels of estrogen tend to have better emotional stability and resilience to stress. When estrogen decreases, you might feel more sensitive or moody, and emotions may feel more intense or harder to control.
Skin Health and Elasticity
Estrogen is closely linked to collagen production and skin hydration. As estrogen levels drop with age, particularly during menopause, you may start to notice changes in your skin. Elasticity diminishes, and skin may become thinner, drier, and less resilient to external stresses. You may also experience increased wrinkles or sagging, especially around the jawline, cheeks, and neck.
Estrogen also promotes the production of hyaluronic acid, which keeps your skin hydrated and plump. When estrogen levels decline, your skin may lose some of that youthful fullness and become more prone to dryness or irritation.
Progesterone: More Than Just a Menstrual Regulator
Progesterone is often seen as the “balancer” hormone, mainly because it works in concert with estrogen to regulate the menstrual cycle and prepare the uterus for pregnancy. However, progesterone does so much more than just that. It's essential for overall health and well-being, especially during perimenopause and menopause.
Sleep Regulation
One of the most impactful, but often overlooked, roles of progesterone is its ability to promote restful sleep. Progesterone has a natural sedative effect on the body and promotes deep, restorative sleep. This is why many women find that they begin experiencing insomnia or more disrupted sleep patterns as their progesterone levels decline in midlife.
Progesterone works by calming the central nervous system, helping you relax and fall asleep more easily. Without enough progesterone, many women struggle with tossing and turning, night sweats, and frequent waking during the night, which significantly affect overall energy levels and mood during the day.
Anxiety Reduction
Progesterone has natural anti-anxiety properties. It works as a mild GABA receptor agonist (GABA is the neurotransmitter that promotes relaxation and a sense of calm). This means that progesterone can help soothe the nervous system and reduce feelings of anxiety or irritability.
When progesterone levels start to drop in perimenopause, many women experience heightened levels of anxiety, restlessness, and irritability, which can be worsened by insomnia or poor sleep. Progesterone’s calming effect helps prevent the overactivity of the nervous system that contributes to these symptoms, promoting a greater sense of emotional balance.
Balancing Estrogen’s Effects
Progesterone and estrogen must be in balance for optimal health. Progesterone counterbalances the stimulating effects of estrogen, ensuring that estrogen doesn’t become dominant or overstimulate tissues, such as the uterus or breast tissue.
In the absence of adequate progesterone, estrogen can become "unopposed," which may lead to estrogen dominance. Estrogen dominance occurs when there’s too much estrogen in relation to progesterone, often resulting in symptoms like heavy periods, bloating, breast tenderness, and mood swings.
Progesterone helps to regulate the menstrual cycle, ensuring that the lining of the uterus sheds properly. Without enough progesterone, the cycle can become irregular, which often leads to more extreme symptoms as the body tries to adjust.
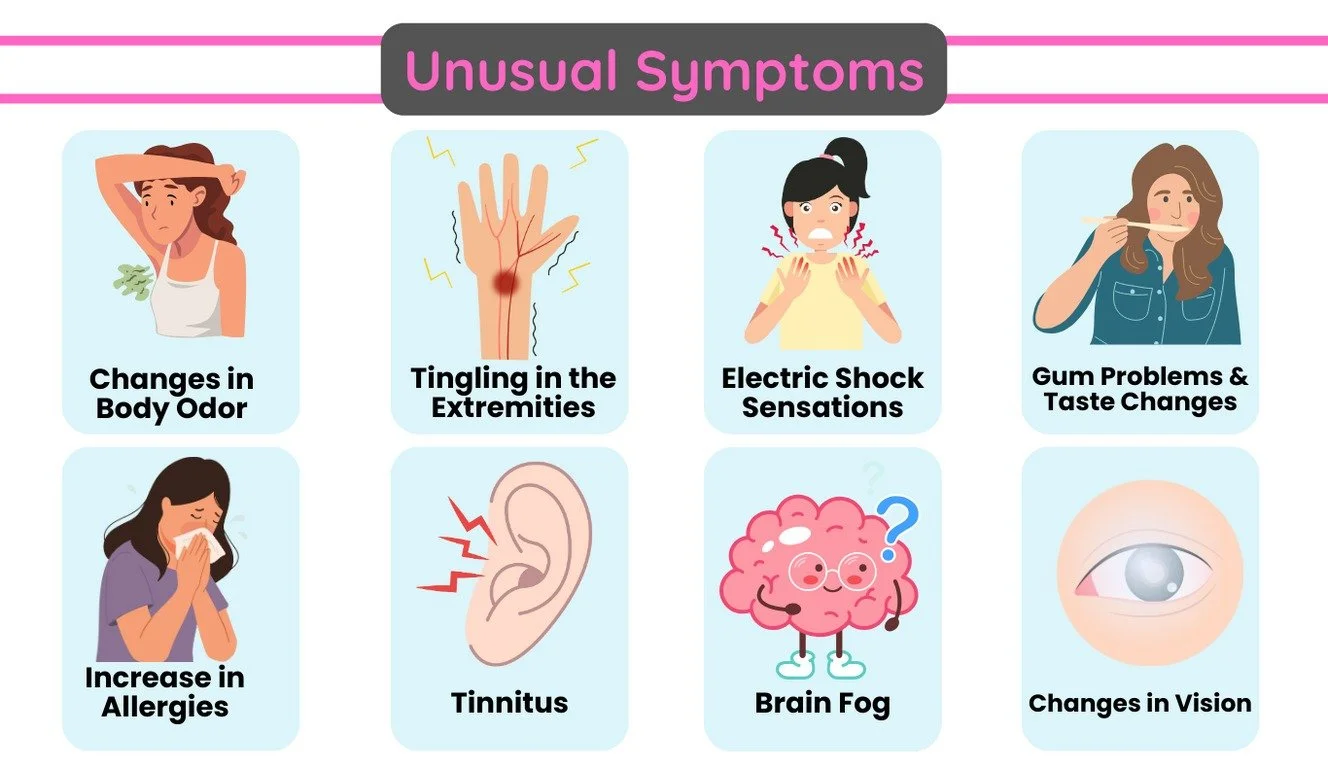
Symptoms No One Talks About
When we think about midlife hormonal changes, we often focus on the obvious symptoms like hot flashes, mood swings, and disrupted sleep. But there are other, less-discussed symptoms that can be just as impactful, and they can leave you feeling confused or frustrated when they pop up.
Joint Pain and Stiffness
If you’ve suddenly started noticing joint pain, especially in your shoulders, knees, hips, or hands, you’re not alone. Estrogen, which plays a role in maintaining healthy cartilage and joint function, drops significantly during perimenopause and menopause. This decline can lead to a variety of musculoskeletal issues, including:
Increased inflammation in the joints, making them feel stiff or painful.
Decreased lubrication in the joints, resulting in discomfort during movement.
Loss of muscle mass, which can strain joints and lead to increased wear and tear.
Changes in Body Odor
This one might surprise you, but body odor can actually change during midlife. Fluctuating levels of estrogen and progesterone can alter the way your body sweats, and in some cases, you may notice a stronger or different scent than usual. Here’s why:
Hormonal imbalances during perimenopause can lead to an increase in sweat production, particularly around the armpits, feet, and groin.
Changes in sweat composition, particularly in the presence of more apocrine sweat glands (the glands responsible for body odor), can make your sweat smell more pungent or different.
Fluctuating estrogen levels can affect the bacterial composition of your skin, which in turn can lead to changes in body odor.
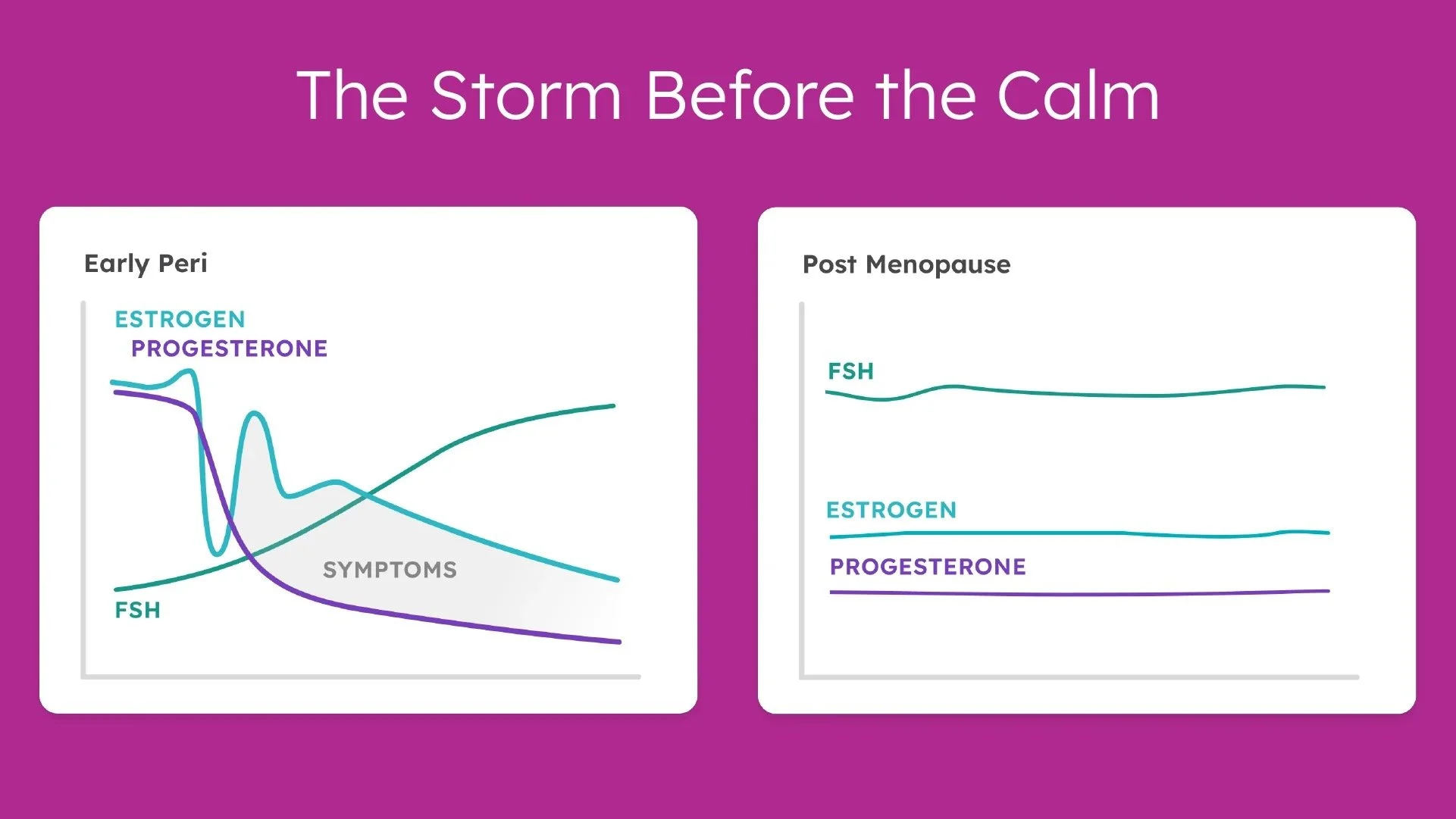
FSH= Follicle Stimulating Hormone
Your Body May Resist Weight Loss
If you’ve noticed that your metabolism seems to be slowing down, you’re not imagining it. Perimenopause can wreak havoc on your body’s ability to maintain a healthy weight. As estrogen levels fluctuate, your body may retain more fat, particularly around the abdomen.
But it’s not all about “trying harder” with diet and exercise. Your body might need a more nuanced approach. Insulin resistance often becomes more prominent during midlife, making it harder for your body to process sugar effectively.
Your muscle mass may also decrease as your estrogen levels drop, which leads to a decrease in resting metabolic rate, meaning you burn fewer calories at rest than you did before. This doesn’t mean the end of your fitness routine. It’s just a sign that your strategy might need a little tweaking, incorporating more muscle-building exercises, eating enough protein, and addressing gut health.
Hormones Impact Your Mood and Mental Health
It’s not just physical changes; hormones can also affect your emotional state. You may have noticed an uptick in irritability, anxiety, or even sadness.
When estrogen levels drop, it can influence the neurotransmitters in your brain, particularly serotonin, the “feel-good” chemical that regulates mood. With less estrogen, serotonin may become less effective, leading to anxiety, depression, or feeling “off.”
The good news is that you're not powerless against this. Balancing hormones, improving your diet (especially by adding mood-supporting nutrients like omega-3 fatty acids, vitamin D, and magnesium), and incorporating stress-reducing activities like yoga or deep breathing exercises can be incredibly helpful.
You need to Prioritize Your Health
Midlife brings hormonal changes that often signal it’s time to re-evaluate how we take care of ourselves. Your body is telling you that it’s time to make your health a priority in ways you may have overlooked before.
Now is the time to stop ignoring fatigue and start listening to your body’s signals. Shift to a more holistic approach that supports your overall well-being. Think of this as an opportunity to finally put your health first and make choices that truly benefit you.
Hormonal Support Can Be a Game-Changer
Bioidentical hormones, lifestyle changes, supplements, and even stress management techniques like meditation or acupuncture can help balance your body in a more natural way.
But the most important piece is personalization. Not every woman will respond to the same treatments or strategies. Working with a healthcare provider who understands hormone health and takes a whole-body approach can be the key to finding the right path for you.
Hormonal Fluctuations vs. Stable Low Levels
One of the most confusing aspects of perimenopause and menopause is the fluctuating nature of hormones. During perimenopause, estrogen and progesterone levels can swing wildly, causing ups and downs in how you feel from month to month, or even week to week. These fluctuations often contribute to a wide variety of symptoms.
But once your hormone levels settle into a low, stable range, many of these symptoms tend to improve or even disappear altogether. This is because your body has adjusted to a new hormonal baseline, which is often referred to as the low-normal level. Let’s explore what this means for you, and which symptoms tend to ease once your hormones stabilize.
When Hormones Settle: Relief from Fluctuating Symptoms
Once your hormones level out after menopause, many of the more erratic symptoms begin to fade. Here’s a look at what you might experience:
1. Joint Pain and Stiffness
As estrogen levels stabilize, the inflammation that was caused by erratic hormone levels may decrease. The pain or discomfort in your joints often starts to feel more manageable, and mobility improves. Although some aches and pains may persist due to aging, many women report that their joint pain diminishes significantly once their hormone levels settle.
2. Mood Swings and Emotional Instability
The emotional rollercoaster you experienced during perimenopause often levels out when your estrogen and progesterone reach a low, stable baseline. Many women find that their mood swings, irritability, and feelings of anxiety subside once the fluctuations settle. While low estrogen can still contribute to feelings of sadness or mild anxiety, the intensity of emotional highs and lows tends to decrease.
3. Hot Flashes and Night Sweats
One of the most bothersome symptoms during perimenopause is hot flashes. Fortunately, these often fade away once your hormones stabilize post-menopause. While a small number of women continue to experience hot flashes even after menopause, for most, the intensity and frequency decrease, leading to better overall comfort and sleep.
4. Body Odor
When estrogen levels fluctuate, sweat production can increase, and the composition of sweat can change, leading to stronger or different body odor. Once hormone levels reach a stable low-normal level, this often improves. Your sweat composition normalizes, and many women notice that their body odor returns to a more familiar state, requiring less management with deodorants or other products.
5. Sleep Disruptions
Sleep problems caused by fluctuating hormones, like waking up in the middle of the night or tossing and turning, often improve once hormonal levels stabilize. Although low estrogen can still contribute to disturbed sleep, the severity of the insomnia tends to lessen once your body adjusts to its new hormone balance.
What to Expect After Hormones Settle
While stabilized low levels of estrogen and progesterone bring relief for many symptoms, it’s important to note that some changes are permanent. For example, as estrogen declines, you may still notice things like:
Thinning hair
Dry skin
Decreased libido
Vaginal dryness
These are not always linked to hormonal fluctuations but to the overall decline in estrogen after menopause. While these symptoms may not completely go away, they can often be managed with the right lifestyle changes, diet, and targeted treatments. For example, vaginal estrogen is a treatment with minimal side effects that can help address issues like vaginal dryness, painful intercourse, urinary urgency, vaginal irritation, and recurrent urinary tract infections.
How to Take Control of Your Midlife Hormones
If you’re tired of feeling like your hormones are in control, it’s time to take charge. Midlife is a time for growth and change. It’s not about battling your body; it’s about learning to work with it.
Here’s how you can start taking control of your hormonal health today:
Get Hormonal Testing: Understand exactly where your hormone levels stand.
Adopt a Balanced Diet: Focus on anti-inflammatory foods, balance your blood sugar, and support gut health.
Move More: Incorporate strength training to maintain muscle mass and boost metabolism.
Manage Stress: Find stress-reducing practices that work for you: yoga, meditation, walking in nature.
Talk to a Professional: Whether it’s a functional medicine doctor, nurse, or coach, find someone who understands how to address hormone balance from all angles.
Hormones aren’t just something you deal with. They’re important signals that can help guide you toward better health in midlife. By tuning into your body’s needs and taking a personalized, holistic approach, you can move through this phase with more ease and balance.
Perimenopause isn’t a decline. It’s a reset. If you’re ready to embrace this transition with balance and vitality schedule a free consultation for a quick chat about your specific needs.