The Gut-Brain Connection: Why Gut Health Affects Your Mind
Did you know that your gut and brain are closely connected, influencing everything from your mood and mental clarity to your stress levels and overall well-being? This connection is known as the Gut-Brain Axis, and is one of the most rapidly evolving areas of health science today.
In this post, we’ll break down what the gut-brain connection is, how it works, and how improving your gut health can have a profound impact on your mind and body.
What is the Gut-Brain Connection?
The Gut-Brain Axis (GBA) is a two-way communication network that links your central nervous system (the brain and spinal cord) with your enteric nervous system (the nervous system of the gastrointestinal tract). While we traditionally viewed the brain as the command center for our thoughts, feelings, and bodily functions, research now shows that the gut plays a major role in influencing our emotions, cognition, and behavior.
How Does the Gut Talk to the Brain?
Communication occurs through multiple pathways:
The Vagus Nerve: A key superhighway of information that directly connects the gut to the brain.
Neurotransmitters: Chemicals like serotonin, dopamine, and GABA, many of which are produced or influenced by gut microbes.
Hormones: Gut bacteria affect levels of cortisol (stress), melatonin (sleep), and others.
The Immune System: Around 70% of immune function is rooted in the gut, meaning inflammation there can have systemic effects, including on the brain.
Key Components of the Gut-Brain Axis
1. Gut Microbiota
Your gut is home to trillions of microbes: bacteria, viruses, fungi, and other organisms collectively known as the microbiome.
These microbes:
Digest food
Produce essential nutrients and neurotransmitters
Regulate immune responses
Maintain the integrity of the gut lining
When a healthy microbiome is disrupted (a state known as dysbiosis), it can throw off everything from mood to metabolism.
2. Inflammation
When the microbiome is out of balance, harmful bacteria can thrive, increasing inflammation and causing conditions like leaky gut, where the intestinal lining becomes permeable and allows toxins to enter the bloodstream.
This triggers systemic inflammation, which can cross the blood-brain barrier and interfere with neurotransmitter function.
Chronic inflammation has been linked to depression, anxiety, and even neurodegenerative diseases like Alzheimer’s.
3. Stress
The relationship between stress and gut health is a feedback loop:
Mental stress alters digestion and gut bacteria composition.
Gut disturbances send distress signals back to the brain, exacerbating anxiety or low mood.
This is why people often feel stress in their gut—as a stomachache, nausea, or appetite changes.
How Gut Health Affects Mental Health
1. Mood Regulation and Anxiety
About 90% of serotonin (a key mood stabilizer) is produced in the gut.
Gut imbalances reduce serotonin availability, increasing the risk of depression and anxiety.
Studies show that people with conditions like IBS (Irritable Bowel Syndrome) are more likely to experience mood disorders, highlighting the gut-brain overlap.
2. Stress Resilience
A healthy gut supports better regulation of the hypothalamic-pituitary-adrenal (HPA) axis, the body's main stress response system.
Balanced gut flora can reduce overreaction to stress and enhance emotional resilience.
Chronic stress, in contrast, can deplete good bacteria, increase gut permeability, and cause systemic inflammation, feeding a vicious cycle.
3. Cognitive Function and Brain Fog
Inflammation and toxin leakage from the gut can interfere with brain function, leading to:
Poor concentration
Memory issues
"Brain fog"
This connection is especially notable in people with autoimmune or chronic digestive disorders, where mental clarity often improves alongside gut healing.
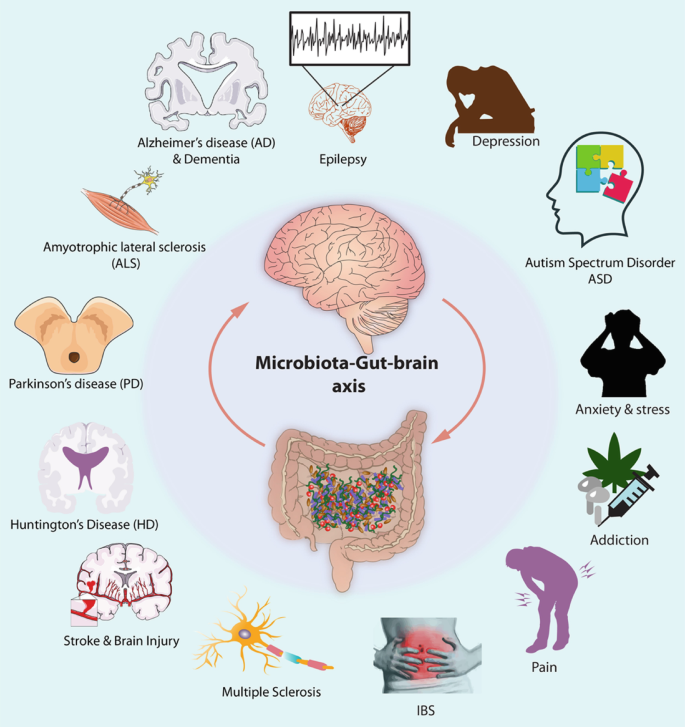
Gut-Brain Axis and the role in Neurological and Psychiatric Disorders
Emerging research reveals that the gut-brain axis, the complex communication network between the gut and the brain, plays a pivotal role in the development and progression of several neurological and psychiatric disorders.
Multiple Sclerosis (MS): In conditions like Multiple Sclerosis (MS), gut inflammation and microbial imbalance may fuel immune system dysfunction and neuroinflammation.
Depression: Depression is now widely recognized as being linked to disruptions in the gut microbiome, which can reduce serotonin production and heighten inflammation.
Parkinson’s Disease: In Parkinson’s disease, early symptoms often begin in the gut, and misfolded proteins may travel from the intestines to the brain via the vagus nerve.
Huntington’s Disease & ALS: In Huntington’s disease and Amyotrophic Lateral Sclerosis (ALS), changes in gut flora and intestinal permeability may exacerbate systemic inflammation and oxidative stress, contributing to neurodegeneration.
Alzheimer’s Disease: Alzheimer’s disease has also been connected to gut-derived toxins and inflammation that impair cognition and memory.
Epilepsy: In epilepsy, certain gut microbes are known to affect seizure thresholds, and dietary strategies like the ketogenic diet are used therapeutically to influence gut-brain chemistry.
Stroke: After a stroke, disruptions in gut microbiota can worsen inflammation and hinder brain recovery, while brain injury itself can impair gut motility and barrier function, creating a vicious cycle.
Irritable Bowel Syndrome (IBS): IBS is long considered a functional gut disorder, is now understood as a gut-brain condition involving hypersensitive nerve signaling, stress, and microbial imbalance, often co-occurring with anxiety or depression.
Autism Spectrum Disorder: Many individuals with autism experience digestive issues, and altered microbiota composition has been linked to behavioral symptoms, possibly through immune and neurotransmitter pathways.
How to Improve Gut Health for a Healthier Mind
Here are practical, evidence-based strategies to nourish your gut and support your mental well-being:
1. Eat a Diverse, Fiber-Rich Diet
A varied diet encourages microbial diversity which is key to a healthy gut.
Focus on whole foods, especially:
Fruits and vegetables (rich in fiber and polyphenols)
Whole grains
Legumes and nuts
2. Include Prebiotics and Probiotics
Prebiotics: Non-digestible fibers that feed beneficial bacteria. Found in:
Bananas
Garlic
Onions
Asparagus
Oats
Probiotics: Live bacteria that help repopulate and balance your microbiome. Found in:
Yogurt
Kefir
Sauerkraut
Kimchi
Miso
You can also consider high-quality probiotic supplements, especially after antibiotics or during high-stress periods.
3. Reduce Stress Naturally
Practice mindfulness, meditation, or deep-breathing exercises to engage the parasympathetic nervous system(rest and digest mode).
Doing these activities regularly can reduce stress and support a healthier gut-brain feedback loop:
Yoga
Walking in nature
Journaling
Creative hobbies
4. Avoid Overuse of Antibiotics
Antibiotics can decimate your microbiome, reducing both good and bad bacteria.
If you must take them, support your gut with probiotics and fermented foods afterward.
5. Exercise Regularly
Exercise increases gut microbial diversity and helps reduce inflammation.
Even light activity like walking, stretching, or cycling enhances digestion and mood.
6. Get Consistent, Quality Sleep
Poor sleep can disrupt your gut flora and vice versa.
Aim for 7–9 hours of restful sleep. Consistent bedtime routines, limited screen time, and reduced caffeine can help.
The gut-brain connection is a powerful and intricate system that affects everything from your mood to your cognitive function. By prioritizing gut health through diet, stress management, and lifestyle changes, you can foster a healthier mind and body.
If you’re struggling with gut issues, brain fog, or mood imbalances, taking a closer look at your gut health may be the key to finding lasting relief.