Why Functional Medicine Works, Even If It Challenges the System
After years working in allopathic care, the conventional medical approach focused on diagnosing and treating symptoms, I began to question whether we were truly helping people heal. I was helping people, yes. But I also saw far too many patients cycle through the system without real answers. Patients were prescribed medications. Symptoms were “managed.” But healing, rarely happened. Even when labs looked “normal,” people still felt unwell.
What Is Functional Medicine?
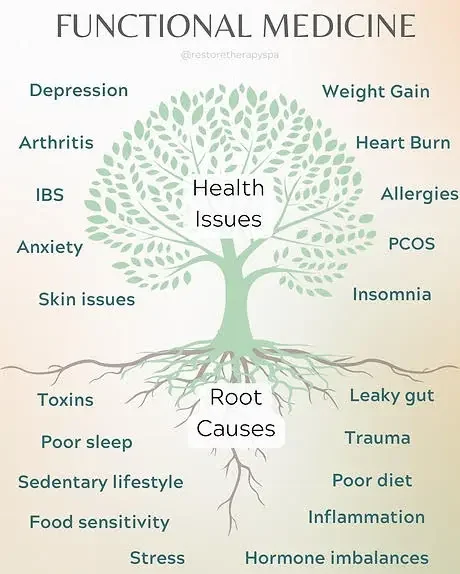
Functional medicine is a patient-centered approach that looks beyond the symptom to uncover why the symptom is happening in the first place. It’s focused on understanding how genetics, lifestyle, nutrition, environment, and stress all interact to impact health.
Where conventional care often asks, “What diagnosis matches these symptoms?” Functional medicine asks, “What’s causing this dysfunction?”
It’s not about replacing conventional medicine. It’s about expanding it. In fact, functional medicine builds on the clinical knowledge I already had as a nurse. Instead of viewing patients through the lens of symptoms alone, I began to see them as whole people whose bodies and stories are deeply intertwined.
What Does Root Cause Really Mean?
Symptoms aren’t just problems to silence, they’re your body’s way of saying something’s off. Your body is always communicating. Fatigue, headaches, bloating, brain fog. They’re signs that something deeper is out of balance.
Let’s say you wake up tired, even after a full night’s sleep. By mid-afternoon, you’re crashing, reaching for coffee, or feeling too drained to focus. You might think, “I just need more energy,” and a conventional approach may offer a quick fix: caffeine or even an antidepressant.
But functional medicine asks: Why is your energy low in the first place? Because fatigue is not a diagnosis. It’s a symptom with many possible causes.
Here are a few:
Iron deficiency or anemia – even a “low-normal” ferritin level can leave you drained.
Thyroid imbalance – especially suboptimal T3 or undiagnosed Hashimoto’s.
Chronic stress or HPA axis dysfunction – when your stress response is stuck in overdrive or burnout.
Poor sleep quality – due to sleep apnea, blood sugar swings, or nighttime cortisol spikes.
Gut dysfunction – imbalances in the microbiome can affect nutrient absorption and inflammation.
Nutrient depletion – especially B12, magnesium, or vitamin D.
Hormonal shifts – from perimenopause to insulin resistance.
In functional medicine, instead of asking, “How can we boost your energy?” we ask:
What’s draining your energy to begin with?
Are your nutrient levels truly optimal, or just “in range”?
Is your sleep restorative, or are you waking up tired?
Is your body constantly reacting to hidden inflammation or stress?
Fatigue is your body waving a flag, asking you to look deeper. And when you do, healing becomes possible.
It’s a shift that turns healthcare from a short-term fix into a long-term, sustainable approach to wellness.
Why Functional Medicine Works?
Functional medicine works because it treats people, not problems.
It offers:
More time: Appointments that last 60+ minutes, not 10.
A deeper lens: Exploring health history, lifestyle habits, and hidden imbalances.
Whole-person care: Including nutrition, sleep, movement, relationships, and emotional health.
Collaboration: Patients are active participants, not passive recipients.
This approach doesn’t always fit neatly into our current medical system, and that’s where the friction lies.
Why the Pushback?
1. It Challenges the Current Model
Conventional medicine is exceptional at acute care, like emergencies, infections, surgeries. But it was never designed for the chronic, complex conditions so many people now face.
Functional medicine asks different questions, and sometimes that makes the system uncomfortable. It suggests that their method may not be enough.
2. It Takes Time
Root-cause care takes time. And time isn’t something most insurance models reimburse well. Functional medicine often requires longer visits, deeper relationships, and out-of-pocket costs, making it harder to scale, but often more effective.
3. It Lives Ahead of the Research Curve
Functional medicine draws on emerging fields like nutrigenomics, microbiome science, and personalized nutrition. Not every protocol is backed by double-blind pharmaceutical trials, but that doesn’t make it unscientific. It often leads where research eventually follows.
4. It’s Deeply Personal, and That’s Hard to Standardize
Functional medicine resists cookie-cutter care. Each patient receives a unique plan based on their root causes. For a healthcare system built on algorithms and protocols, this flexibility can feel like chaos. For the patient? It often feels like the first time someone truly listens.
As a nurse, functional medicine gave me the framework and tools to truly help people heal, not just manage or mask their symptoms.
What I Wish Nursing Had Taught
If I could go back to nursing school, I wouldn’t erase what I learned. Acute care saves lives. But I do wish we were also taught:
That symptoms often reflect deeper imbalances, not just issues to silence
That food, stress, and lifestyle are central to health
That a “normal” lab doesn’t always mean a healthy patient
That true healing requires time, curiosity, and compassion
Functional medicine expanded my view of what’s possible in care. It made me a better nurse, not because I abandoned the system, but because I saw where it could grow.
Functional medicine works, even if it challenges the system. It works because it asks better questions. Because it treats root causes, and sees the patient as a whole person. The future of care isn’t one model over the other, it’s integration. And the more we can blend the strengths of conventional medicine with the depth of functional care, the better off patients will be. Functional medicine disrupts the norm, but maybe that’s exactly what healthcare needs right now.
If you’re living with symptoms that don’t have clear answers, or if you feel like your concerns aren’t being heard, know that you’re not alone. Let’s explore what your body might be trying to say. Reach out. I’d love to help.